Innovation in Social Services
Rooted in equity, Felton Institute transforms quality of life and promotes social justice to accelerate community led change.
Our Programs
Latest News
Kamala Harris, Fearless Leader for Criminal Justice Reform
Vice President Kamala Harris is to be commended for initiating a criminal justice diversion...
Felton Honors Board Vice Chair Tamara Steele for Women’s History Month
Felton Institute Board Vice Chair Tamara Steele recalls, "My mom said that I was always the...
Eve Meyer Shines a Light on Suicide Prevention
“I had this feeling of coming home,” Eve Meyer, former executive director of San Francisco Suicide...
ECE REACH Apprenticeship: Empowering Dreams, Transforming Communities!
“When a child can connect with their teacher in their native language, Spanish, and with someone...
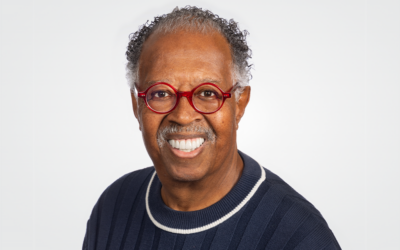
Black History Month: A Message from Al Gilbert, President and CEO of Felton Institute
Celebrating Black History Month is an acknowledgment of the rich history and many contributions of...
Felton Board Chair Dr. George Woods on Forensic Psychiatry and the Criminal Justice System
“When we talk about different groups, whether gender, identity, or ethnicity, we must also talk...